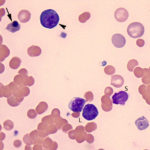
Nucleated RBC are usually not seen in the blood of healthy mammals (low numbers may be seen in dogs and camelids, but are rarely normally seen in other species). The most common type of nRBC seen in blood is the fully hemoglobinized or orthochromic metarubricyte (a cell with red cytoplasm and a small pyknotic nucleus). However, polychromatophilic metarubricytes and even earlier stages (basophilic rubricyte, which has purple to blue-purple cytoplasm and a somewhat viable nucleus) may be seen in blood as well, depending on the cause. When nRBCs are increased in blood, it is called a normoblastosis, erythroblastosis or metarubricytosis (the latter is the least preferred term as it only refers to the most mature form of nucleated RBC – the metarubricyte – when even earlier forms may be seen as well).
Nucleated RBCs are most often noted in dogs, cats and camelids in the context of strongly regenerative anemia. However, even in the latter context, it is unclear that they are “part” of the regenerative response or reflect other changes, such as alterations to bone marrow sinusoids (see more below). They are seen less often in regenerative anemia in cattle and rarely seen in horses, even those with a strongly regenerative anemia. Nucleated red blood cells can also be observed in blood smears from non-anemic sick camelids or camelids with non-regenerative anemias, sometimes in high numbers. Thus, nucleated red blood cells by themselves should not be used to judge whether an anemia is regenerative or not in any species. They can be seen in increased amounts in blood in other conditions, including lead poisoning, altered or abnormal splenic function, or bone marrow hypoxia or injury (suspected mechanism in heat stroke). It has long been postulated that a normoblastosis in blood of animals with a regenerative anemia is part of the regenerative response or an expected response to an anemia, however this may not be true. In reality, we do not know why we see nRBCs in circulation in some animals with a regenerative anemia. It may be due to the type, severity or cause of anemia, since more nRBCs are seen, for instance, in dogs with a hemolytic anemia (such as due to regenerative variants of immune-mediated hemolytic) than dogs with experimental blood loss. It is possible that nRBCs in blood in animals with regenerative anemia reflects an altered bone marrow microenvironment (e.g. defective pitting function of marrow macrophages, which control, to a certain degree, the enucleation of developing red blood cells or an altered sinusoidal endothelial barrier, such as from hypoxia) or altered splenic function (where presumably circulating nRBC are removed once they are expelled from marrow).
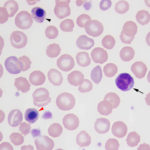
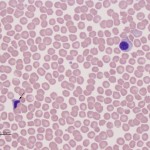
Nucleated RBC must be distinguished from lymphocytes, which they can closely mimic in blood. In fact, hematologic analyzers frequently count nRBC as lymphocytes resulting in inaccurate automated differential leukocyte counts and a measured “WBC” count. When nRBC are present in blood, they are included in the measured “WBC” count and the WBC count must be corrected for the number of nRBC. For more information on this and causes of increased nRBC in blood, refer to the nRBC test page. In fact, the human eye is better than the machine because we can pick up features in the cells, which help us distinguish between these cell types. Features that are typical of nRBC are:
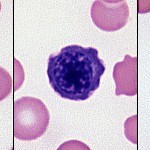
- Nuclear chromatin: As RBC precursors mature in the marrow, their nuclei become smaller (as do the cells) with successive division and becomes apoptotic, so the nuclear chromatin becomes more and more condense (smooth dark). In contrast, lymphocytes have a mixture of euchromatin and heterochromatin, giving them a “lighter” and not “condensed” chromatin pattern.
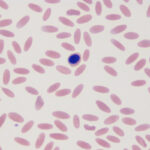
- Cytoplasm color: Metarubricytes have large amounts of hemoglobin in their cytoplasm, which imparts a red color to the cell, just like a normal RBC. Nuclei are quite pyknotic (condensed chromatin) in such cells. More immature nRBC have RNA which imparts a blue color to the cytoplasm. If hemoglobin is concurrently being produced in the cell (polychromatophilic rubricyte stage), the cytoplasm will be purple (resembling a polychromatophil). If hemoglobin is not being produced (e.g. basophilic rubricyte), the cytoplasm can be quite dark blue. The latter can resemble a lymphocyte, particularly a reactive lymphocyte, but the nuclear features are more condensed than a lymphocyte.
- Cytoplasmic features: nRBC may contain chunks of RNA, i.e. basophilic stippling, but this is not a feature of all nRBC.
- Cytoplasmic borders: They tend to be more ruffled than a lymphocyte.
Context also helps…we do not expect to see many nRBC in healthy animals, non-anemic animals or animals with no evidence of a regenerative response (sick camelids are an exception to this). In the setting of a regenerative anemia, we may expect to see some nRBC (see above for caveats).
Nucleated RBC must also be distinguished from apoptotic white blood cells (WBC). Apoptotic cells can be due to storage of blood or may be seen in fresh blood in animals with heat stroke or drugs that cause apoptotic or oncotic death of WBC. It can be difficult to differentiate the two but essentially the cytoplasm of the apoptotic cell mimics the cell of origin. For neutrophils (which usually die the quickest), the cytoplasm is colorless to light pink and may contain granules. In contrast, the nRBC should have smooth uniform red, purple (or infrequently blue) cytoplasm.
Related links
- nRBC gallery in Atlas
- Hematology album in Atlas
- nRBC test page: Causes of a high nRBC in blood.
