Agglutination
Agglutination refers to the phenomenon where red blood cells stick together in three-dimensional clumps. Agglutination is due to the binding of antibodies to red blood cells. When single antibodies bind to more than one blood cell, agglutinates form. Agglutination is usually a pathologic finding and supportive of a diagnosis of immune-mediated hemolytic anemia (IgM antibodies, which are multivalent, are more likely to form agglutinates), however there are some non-pathologic causes of agglutination. Causes are:
- Immune-mediated hemolytic anemia (IMHA): Agglutination is suspected due to multivalent IgM, or rarely divalent IgA, antibodies. IgG anti-RBC antibodies do not usually cause agglutination.
- EDTA pseudo-agglutination: EDTA can unmask hidden epitopes in RBC. Animals that have naturally occurring antibodies to these epitopes can bind to the RBC causing agglutination. This may erroneously lead to a diagnosis of IMHA, however affected animals are not usually anemic (unlike IMHA). This has been reported in a cat (Schaefer et al., 2009).
- Drugs: Heparin can induce agglutination of horse RBC.
Rouleaux formation
Rouleaux formation is a term describing groups of red blood cells that form stacks, such as stacks of coins. This is a normal finding in the blood of healthy horses and to a lesser extent cats, but is not normally seen in dogs or cattle (in health or disease). Horse red blood cells are thought to form rouleaux because they have decreased negative charge (altered zeta potential) on their red blood cells. Rouleaux can also be a marker of underlying disease, even in the horse and cat (rouleaux formation can be excessive, i.e. greater than expected, in these species). Excessive rouleaux formation in any species indicates hyperglobulinemia. Note that a low albumin will promote rouleaux formation (but not cause it). Increases in two types of globulins results in rouleaux formation:
- Fibrinogen: This is a β-2 globulin and an acute phase reactant, i.e. values increase with inflammation. High fibrinogen is also a feature of renal disease in the horse and cat.
- Immunoglobulins: These proteins, which migrate in the β or γ regions of an electrophoretogram, can increase under reactive or neoplastic conditions
- Reactive: Inflammation or antigenic stimulation. A polyclonal gammopathy is expected.
- Neoplastic: Neoplasms of B lymphocytes or plasma cells, e.g. B cell lymphoma, B cell chronic lymphocytic leukemia, extramedullary plasmacytoma, solitary plasma cell tumor of bone, multiple myeloma. A monoclonal gammopathy may be seen with these neoplasms.
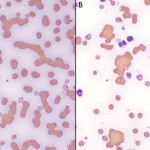
Agglutination versus rouleaux formation
Agglutinates can sometimes be distinguished from rouleaux by their characteristic appearance on blood smears (agglutination forms three-dimensional clusters, whereas rouleaux forms stacks), however this can be difficult with severe rouleaux. Similarly, a slide agglutination test cannot reliably distinguish between agglutination and severe rouleaux formation. The best way to distinguish between these two phenomena (with important consequence for diagnosis and patient care) is to perform a saline dilution test, which is also called a saline dispersion test. This is done by placing one drop of blood to 4 drops or as high as 10 drops of isotonic saline (0.9% NaCl), i.e. a 1:4 or 1:10 dilution of blood to saline) and then examining the dilution as a wet mount (similar to that done for urine sediments, i.e. place a drop of the dilution on a slide, add a coverslip and then examine it with the iris diaphgram of the microscope closed or the microscope condensor down to increase contrast). Saline dilution will disperse rouleaux but not agglutination (unless the agglutination is caused by low avidity antibodies, particularly if the dilution is left sitting too long before examination or if the RBCs are washed before examination).
