Interpretation
Reactive bone with evidence of osteolysis
Moderate mixed inflammation (neutrophils, macrophages)
 |
 |
 |
 |
Explanation
Given the radiographic findings, the differential diagnoses should include both neoplastic and reactive conditions, as radiographs alone do not reliably differentiate between primary tumors, metastatic tumors, or osteomyelitis1 (Question 1). The initial radiology report listed metastatic carcinoma, primary bone tumor, and osteomyelitis as differential diagnoses, in that order. A primary bone tumor was considered clinically less likely given the breed and location of the lesion; as the lesion was slightly towards the middle of the humerus, raising the index of suspicion for metastatic neoplasia.
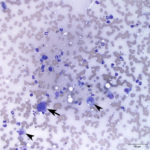
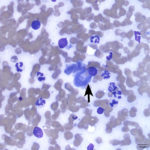
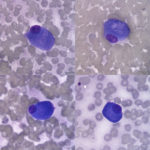
Overall the specimen was of moderate cellularity consisting of mostly individualized osteoblasts (Figure 3) with few osteoclasts (Figure 4) on a proteinaceous background with a large amount of blood and platelet clumps. The osteoblasts were well-differentiated and oval with moderate amounts of deep blue cytoplasm with a pink grainy hue in a perinuclear location. The nucleus was oval, eccentric, and often oriented perpendicular to the axis of the cell. The chromatin was coarsely stippled with 1-3 small, indistinct nucleoli. Anisocytosis and anisokaryosis were mild. The osteoclasts included few mature, multinucleated forms, as seen in Figure 4, but also immature forms, as shown in Figure 1. The immature osteoclasts were smaller with 1-2 nuclei and magenta grainy cytoplasm. One of the smears also contained leukocytes in numbers considered excessive for the amount of blood present (Figures 1 and 2). The inflammatory cells were present individually and in a single large dense aggregate with nuclear streaming. The inflammatory cells included predominantly non-degenerate neutrophils with fewer vacuolated macrophages. No infectious agents were seen. Given the sample cellularity, inflammation, and morphologic appearance of the osteoblasts lacking cytologic criteria of malignancy, the sample was interpreted as reactive bone with inflammation, rather than a neoplastic process (osteosarcoma) (Question 2). Infectious disease testing (e.g. fungal and bacterial cultures) were recommended to determine an underlying cause for the inflammation (Question 3). Surgical biopsy with histopathologic examination would also be prudent, particularly if cultures are negative.
Follow-up
Due to the radiologist’s differential of a metastatic carcinoma, an abdominal ultrasound was performed. No mass lesions were identified on ultrasound or on thorough physical examination. A surgical biopsy of the bone lesion was performed approximately one month after the initial radiographic and cytologic examinations were performed. The histopathologic interpretation was reorganized / remodeled bone. It was commented that the findings were not specific as to the underlying etiology. There was no evidence of inflammation, infection, or neoplasia. The dog re-checked at CUVS one month after the biopsy for repeat radiographs. The radiographs revealed substantially thickening of the cortex with no evidence of osteolysis. The findings were interpreted as continued remodeling of the previously noted lytic lesion. There was no evidence of an underlying aggressive osseous lesion. No definitive cause for the bone lesion was ever identified. No further diagnostics were pursued given the clinical resolution of the lameness and radiographic resolution of the bone lesion.
Discussion
The majority of aggressive bone lesions in dogs are malignant tumors, with osteosarcoma representing the most common primary bone tumor, which typically affects the appendicular skeleton.2 Other examples of primary bone tumors include chondrosarcoma, fibrosarcoma, and hemangiosarcoma. Bones, particularly ribs, vertebrae, and proximal long bones, can also be affected by metastatic neoplasia.1 Carcinomas are much more likely to metastasize to bone than sarcomas, and tissues of origin include mammary, thyroid, prostate, ovary, and lung.1,2 Bone marrow tumors (e.g. plasma cell tumor, lymphoma) and tumors with local invasion into bone (e.g. squamous cell carcinoma) can also result in bone lysis and proliferation.3 There are also uncommon benign bone tumors, which primarily affect the skull bones.1 Non-neoplastic bone lesions are less common and include inflammatory, cystic, and proliferative lesions.2–4 Osteomyelitis can be due to bacterial (e.g. Actinomyces, Nocardia, Staphylococcus, Streptococcus), less frequently fungal (e.g. Coccidiodes, Blastomyces, Cryptococcus, Histoplasma, Aspergillus, Geomyces), and rarely protozoal (Hepatozoon) agents.1,3,5 Bacterial osteomyelitis is rarely due to hematogenous spread in the dog, whereas fungal infections typically are hematogenous following spore inhalation.1 Bacterial osteomyelitis is more often a complication of compound fractures, wound contamination during open fracture repair, bite wounds, or gunshot injury.1
To further investigate the underlying cause of an aggressive bone lesion, cytology and/or histopathology can be pursued. In a recent retrospective of 68 bone lesions in dogs, the accuracy of cytologic examination of fine needle aspirates (83%) was similar to that of histopathologic examination of incisional biopsies (82.1%).2 The accuracy was also similar for diagnosis of tumor type (50% cytology and 55.5% histopathology).2 Perhaps most importantly in this study, a benign lesion was never misdiagnosed as malignancy on cytology.2 An earlier study looked at the diagnostic agreement between cytology and histopathology. The agreement was far higher in cases of neoplastic (92%) than non-neoplastic (27%) lesions.4 Not surprisingly, there was higher concordance when the sample cellularity on cytology was high.4
Healthy, normal bone consists of abundant osteoid matrix with low numbers of osteoblasts, osteoclasts, chrondrocytes, and periosteal cells.3,5 Aspiration of normal, intact bone is difficult and is expected to be poorly cellular.3 With bone pathology, regardless of the etiology, the cellularity is increased, as the formation of new bone is a common response to injury.1,5 The radiographic appearance of aggressive bone lesions is a balance between proliferative and lytic areas, therefore increased numbers of osteoblasts and osteoclasts are expected findings.1 Aspirates of tumors are typically more cellular than reactive bone.3 Reactive bone refers to a non-neoplastic proliferation of osteoblasts in response to bone injury, which can be secondary to trauma, inflammation, or underlying neoplasia.1,3 Histologically, reactive bone consists of spicules of unmineralized osteoid and trabeculae of woven bone lined by a single layer of plump osteoblasts.1 Cytologically, reactive osteoblasts (as shown in Figure 3) have deep blue cytoplasm with a perinuclear clearing, due to abundant rough endoplastic reticulum and prominent Golgi apparatus, respectively.3 They have a low nuclear to cytoplasmic ratio, are smaller and more uniform in appearance, and lack nuclear features of malignancy as compared to neoplastic osteoblasts in cases of osteosarcoma.5 If there is a question between reactive and neoplastic osteoblasts, histopathologic examination should be pursued to evaluate tissue architecture. As with any cytologic sample, a poorly cellular sample should raise concern that it may not be diagnostic or fully representative of the lesion. Most osteosarcomas arise from within the medullary cavity, therefore a shallow aspirate could yield low numbers of reactive osteoblasts only.1 It is also important to note that the cytochemical stain alkaline phosphatase (ALP), will be positive in both reactive and neoplastic osteoblasts, and should not be used to make this distinction.3 ALP staining is helpful in cases when a cytologic diagnosis of sarcoma has been made, but the cell of origin is unclear. ALP staining has a sensitivity of 100% and specificity of 89% in the diagnosis of osteosarcoma.6 Reported false positives include chondrosarcoma, amelanotic melanoma, and multilobular tumor of bone.6
Cytology is an excellent first step in the diagnostic work-up of aggressive bone lesions, as it minimally invasive with a quick turnaround time. As with any diagnostic test, it is important to understand its utility and limitations. Additionally, providing a signalment and complete history including physical examination abnormalities, description of the sampled site, and the results of imaging and other diagnostics are key in helping the pathologist(s) reach an accurate diagnosis.1 This case highlights the cytologic appearance of reactive osteoblasts in a rare case of reactive bone, confirmed histopathologically, radiographically, and clinically.
References
- Thompson K. Bones and Joints. In: Maxie MG, editor. Jubb, Kennedy, and Palmer’s Pathology of Domestic Animals. Fifth edit. Philadelphia: Saunders Elsevier; 2007. p. 92–130.
- Sabattini S, Renzi A, Buracco P, Defourny S, Garnier-Moiroux M, Capitani O, et al. Comparative Assessment of the Accuracy of Cytological and Histologic Biopsies in the Diagnosis of Canine Bone Lesions. J Vet Intern Med. 2017;31(3):864–71.
- Barger AM. Cytology of Bone. Vet Clin North Am – Small Anim Pract [Internet]. 2017;47(1):71–84. Available from: http://dx.doi.org/10.1016/j.cvsm.2016.07.005
- Berzina I, Sharkey LC, Matise I, Kramek B. Correlation between cytologic and histopathologic diagnoses of bone lesions in dogs: A study of the diagnostic accuracy of bone cytology. Vet Clin Pathol. 2008;37(3):332–8.
- Fielder SE. The Musculoskeletal System. In: Valenciano AC, Cowell RL, editors. Cowell and Tyler’s Diagnostic Cytology and Hematology of the Dog and Cat. Fourth edi. St. Louis: Elsevier Mosby; 2014. p. 216–8.
- Barger A, Graca R, Bailey K, Messick J, De Lorimier LP, Fan T, et al. Use of alkaline phosphatase staining to differentiate canine osteosarcoma from other vimentin-positive tumors. Vet Pathol. 2005;42(2):161–5.
Authored by: A. Newman
