Vitreous humor from a horse
Case information
A 16 year old Icelandic horse gelding presented with a two month history of periocular and perioral alopecia, generalized pruritus, hypersensitivity to touch, weight loss and bilateral uveitis leading to recent blindness. The patient was treated prior to presentation with topical 1% atropine, topical 0.1% dexamethasone ophthalmic and systemic non-steroidal anti-inflammatory medications. The treatment alleviated the signs of ocular discomfort but signs recurred immediately each time treatment was discontinued. The horse was imported from Iceland six years prior to admission, was used as a pleasure horse, and in 6 years of current ownership had never traveled outside of the northeastern United States. Seven other horses on the farm were reported to be healthy and in good body condition.
On presentation a routine physical examination was unremarkable except for periocular and perioral alopecia, abnormally low body condition score (3/9), and the following ocular changes:
Bilateral: Absent menace, pupillary light and dazzle reflexes with intact palpebral reflexes
Right eye: Chronic uveitis with phthisis bulbi, fibrinoid aqueous humor, secluded pupil, posterior synechiae and loss of corpora nigra
Left eye: Markedly hypotonic, yellow-green color to the aqueous humor and moderate flare, diffuse posterior synechiae, similar iris changes to the right eye
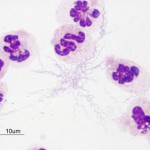
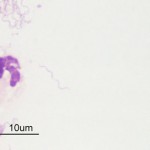
A complete blood count was performed and showed an inflammatory leukogram. A chemistry panel was unremarkable. Humane euthanasia was elected because of quality of life issues related to the severe pruritus, weight loss, persistent ocular pain and blindness. Vitreous and aqueous humor samples were obtained from both eyes immediately following death and submitted for cytologic analysis (see Figures 1 and 2 for representative images of the vitreous samples) and a complete necropsy was performed.
View the following photomicrographs and answer the following questions:
- Characterize the inflammation in the right and left vitreous (Figures 1 and 2).
- Can you identify the etiologic agent?
- What are your differential diagnoses for this agent?
- What further testing would you recommend for confirmation?
 |
 |
Answer on next page
