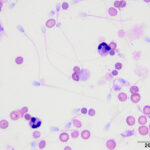
Peritoneal fluid from a dog
Case information
A 1-year-old intact male dog was presented on an emergency basis to the Cornell University Hospital for Animals (CUHA) after a blunt traumatic episode. The dog was quiet, alert and responsive upon physical examination. Multiple cutaneous abrasions were noted around the right hind leg and inguinal region. The mucous membranes were tacky and pale pink. The dog was tachycardic (190 beats per minute) and no overt murmurs or arrhythmias were auscultated. Decreased bronchovesicular sounds were auscultated bilaterally, but there were no crackles or wheezes. The dog was ambulatory in the front legs with paraparesis of the hind legs due to multiple pelvic fractures, which were confirmed on lateral and ventrodorsal radiographs. There was a bloody preputial discharge and hematuria.
Abbreviated blood work performed in-house revealed a mild hyperglycemia (136 mg/dL; reference interval [RI]: 60 – 120 mg/dL) and hyperlactatemia (4.4 mmol/L; RI: < 2.0 mmol/La) with a normal hematocrit (45%; RI: 41 – 58%) and total solids (7.2 g/dL; RI: 5.9 – 7.8 g/dL). Initial abdominal FAST scan ultrasound showed no abnormalities. A repeat heparinized plasma biochemical analysis, performed after treatment and fluid therapy, showed a persistent hyperglycemia (167 mg/dL; RI: 68 – 104 mg/dL) and mild increases in aspartate aminotransferase (AST: 103 U/L; RI: 18 – 56 U/L) and creatine kinase (CK: 3760 U/L; RI: 64 – 314 U/L) activities. There were no evidence of azotemia (urea nitrogen: 21 mg/dL [RI: 9 – 26 mg/dL]; creatinine: 0.8 mg/dL [RI: 0.6 – 1.4 mg/dL]). Approximately 15-hours post-hospitalization, there was a small amount of abdominal fluid. The fluid was aspirated into an EDTA (purple top) tube and submitted to the laboratory for peritoneal fluid analysis.
Provided are the results and representative images from direct and cytospin smears of the peritoneal fluid.
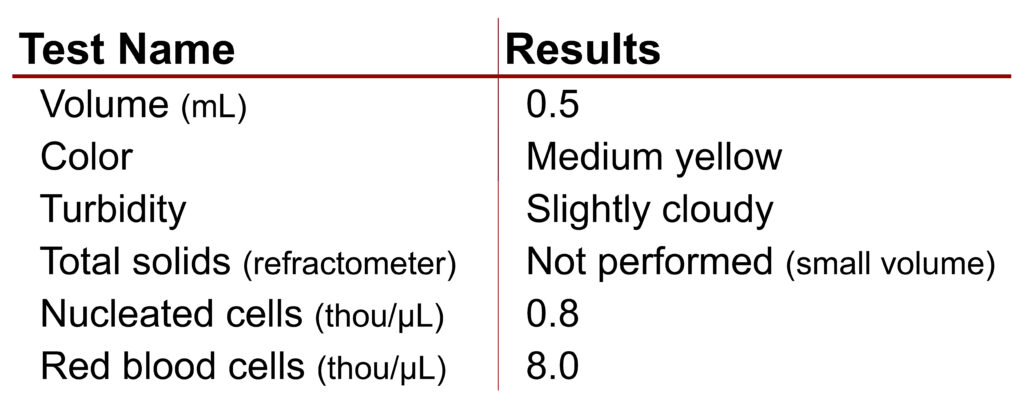 |
Using the provided information answer the following questions,
- What is the predominant cell population in the sample?
- What is your cytologic diagnosis?
- What additional test could be considered to further support your diagnosis?
Answers on the next page.
Footnote
a: Mathews, K.A. (2012). ‘Monitoring Fluid Therapy and Complications of Fluid Therapy’, in DiBartola, S.P. Fluid, Electrolyte, and Acid-Base Disorders in Small Animal Practice. St. Louis, Missouri: Saunders Elsevier Inc. pp:386–404.