
On the other hand, a major challenge is to discriminate between reactive lymphocytes and neoplastic hematopoietic cells (generally called ‘blasts” because their lineage is uncertain, i.e. they could be myeloid or lymphoid in origin). This decision is based on several findings, including the features of the cells, their numbers in blood, and clinical and hematologic data from the patient as outlined in the table below. When in doubt, clinical pathologists “fence sit”, i.e. they may write a lengthy description of the cells and not decide if they are reactive lymphocytes or neoplastic cells. In those circumstances, finding a reason for the presence of these cells in blood is indicated (i.e. look for hematopoietic neoplasia in other sites, including the skin) or, if no reason is found, repeat testing to see if the finding is persistent. Reactive lymphocytes usually are a transient finding in blood, particularly if the primary disease process has been resolved. Note, that some people use the term “atypical lymphocytes”. At Cornell University, we avoid this term because it is of uncertain meaning and uninformative. We prefer to decide if the cells are neoplastic or reactive or if we need to “fence sit”, then we just provide a comment describing our thoughts on the cells in blood.
Note, that it is difficult to precisely classify an individual cell, unless there are others with similar features to compare it to. Contrasting a cell to the “company it keeps” or others like it is crucial in helping us lean towards or be definitive for a reactive cell versus cancer. If there are rare cells of concern in blood, we are not going to lean or be definitive in most cases and will absolutely sit the fence – it could go either way (be reactive or cancer) – this is despite showing only one cell in the image below. The smears these were taken from had enough other cells for us to make the distinction and note the term “likely” in the header.
For additional information (and images) on differentiating reactive from neoplastic cells in blood, see related links.
| Likely reactive | Likely neoplastic* | |
| Feature | 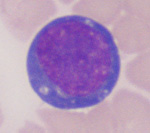 |
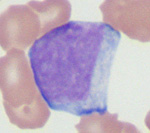 |
| Overall comparing to other cells | Variable in cell size, cytoplasmic features (amount, color, granule presence), nuclear size, nuclear shape, nuclear to cytoplasmic ratio; variability supports multiple versus one clone | More alike (from one clone) than different but not identical (in those features listed for reactive cells) |
| Chromatin | Clumped (heterochromatin) | Fine (euchromatin): Actively transcribing cell |
| Nucleoli | Absent | May be present |
| Cytoplasm | Deep smooth blue (increased RNA as producing protein), variable in amount, color, and content | Can be grainy blue, may be lighter or darker than normal or less scant than normal, more uniform content |
| Clinical features | Young animals, no evidence of lymphoma or leukemia | Usually (but not always) older; lymphadenopathy or organomegaly (spleen, liver usually); mild to moderate lymphadenopathy or organomegaly can be seen with acute leukemia arising in the marrow) |
| Hemogram results | Usually no other cytopenias, unless related to underlying disease that is causing antigenic stimulation | Other cytopenias if acute leukemia (myeloid or lymphoid), may be no other cytopenias or mild cytopenia if lymphoma |
| *Cells are called blasts so as not to presume their origin (blasts could be any hematopoietic lineage in an acute leukemia or could be derived from a large cell lymphoma; see leukemia types). | ||
Related links
- Reactive lymphocytes: Additional image of neoplastic hematopoietic cells (blasts) versus reactive lymphocytes.
- Leukemia: Definitions, types and the tools we use for distinguishing between them.
