Lots of terms are thrown around hematologic testing (and clinical pathology in general) and some terms mean different things, depending on the context in which they are applied. A classic example is the term myeloid, which means all non-lymphoid cells (granulocytes, monocytes, erythroid cells, megakaryocytes) in the context of acute leukemia, whereas it means all granulocytes and monocytes when referring to a myeloid to erythroid ratio in marrow. Confusing!
Below is a list of terms and definitions used routinely in hematologic testing.
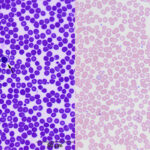
- Routine hematologic stains: Blood smears are stained with Romanowsky type dyes, including a modified Wright’s stain (used in the Clinical Pathology Laboratory at Cornell University) and rapid stains, e.g. Diff-quik®. These stains consist of acidic (red) and basic (blue) dyes. In smears, nuclei and RNA stain blue whereas hemoglobin in red blood cells (RBC) stains red.
- Reticulocytes: These are immature anucleate RBC in which the RNA in the cytoplasm has been precipitated with a supravital dye (e.g. new methylene blue) or stained with a fluorescent dye (e.g. thiazole orange) for laser detection. At Cornell, reticulocytes are identified and quantified by their absorption of a nucleic acid-binding dye, Oxazine-750. We use these techniques to quantify the number of immature anucleate RBC in blood, which is expressed as the reticulocyte percentage (of all RBC). This quantification is only done routinely only in dogs and cats. There are two types of reticulocytes – aggregate and punctate – which are distinguished by the amount of RNA in their cytoplasm (as seen in a new methylene blue-stained smear).
-
- Aggregate reticulocytes contain a large amount of RNA, which precipitates as chunks or aggregates in immature anucleate RBC in new methylene blue-stained smears. These correspond to polychromatophils on a routinely stained blood smear, i.e. all polychromatophils are (aggregate) reticulocytes. After aggregate reticulocytes are released from the bone marrow, they are thought to mature to punctate reticulocytes, which then mature or are remodeled in the spleen to normal sized (normocytic) RBC.
- Punctate reticulocytes contain small amounts of RNA, which are seen as small blue dots in immature anucleate RBC in new methylene blue-stained smears. Punctate reticulocytes contain too little RNA to be polychromatophilic on routinely stained smears (i.e. they are red not purple and are thus not called polychromatophils). They may be larger than mature RBCs (i.e. they can be, but are not always, macrocytes).
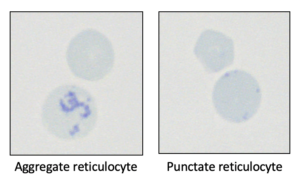
Reticulocytes (new methylene blue)
- Polychromatophilic erythrocytes/polychromasia: RBCs that have a blue-ish or purple tinge to their cytoplasm in routinely stained blood smears (Wright’s or Diff-quik stains) are called polychromatophilic RBC or polychromatophils. These cells correspond to immature anucleate RBC that contain a lot of RNA (in the form of ribosomes and polyribosomes) in their cytoplasm (the blue of the RNA offsets the red of hemoglobin creating the purple color). These immature cells often appear larger than normal RBC in the blood smear. They correspond to aggregate reticulocytes on a new methylene blue-stained smear, i.e. all polychromatophils are (aggregate) reticulocytes. The number of these immature RBC is subjectively quantified in Wright’s-stained blood smears as mild, moderate or marked polychromasia.
- Macrocytes: These are RBC that appear larger than normal in routinely stained blood smears but are the same color as a mature RBC (i.e. red or normochromic). Macrocytes can be immature RBC that contain no or small amounts of RNA in their cytoplasm. If they contain a little RNA that can be precipitated, they would correspond to punctate reticulocytes in a new methylene blue-stained smear. However, some immature anucleate RBC are larger than mature RBC but contain too little RNA to be detected in a new methylene blue-stained smear or fluorescent dyes (and would not be called reticulocytes). Macrocytes can also be produced through other mechanisms, e.g. cell swelling or abnormal RBC production. In these situations, macrocytes do not correspond to punctate reticulocytes in a new methylene-blue stained smear. Thus, macrocytes may or may not be punctate reticulocytes.
- Nucleated red blood cells (nRBC): These are immature erythrocytes, which have still retained their entire nuclei. Note that all RBCs (immature and mature) contain nuclei in non-mammalian species (e.g. birds, amphibians, reptiles).
- Howell–jolly bodies: These are nuclear fragments within RBC and are also called micronuclei. RBCs that contain these nuclear fragments are not called nRBCs.
- Hemolysis: The meaning of this term is context-dependent.
- General context: The term hemolysis invokes the mental picture of lysed or ruptured RBCs. Rupturing of RBCs can occur in vitro or as an artificial phenomenon due to problems with sample collection, storage and handling (in vitro hemolysis). The released hemoglobin then acts as an interferent, affecting results of other hematologic and biochemical tests. Rupturing of RBCs can also occur in vivo within blood vessels as a pathologic condition (see below).
- In the context of anemia: The term hemolytic anemia or hemolysis as a mechanism of anemia refers to accelerated destruction or removal of RBCs in vivo or reduced RBC lifespan from premature destruction. Therefore, the concept of hemolytic anemia and the types of hemolytic anemia (extravascular and intravascular hemolysis) may be easier to understand if you think of the term hemolysis to simply mean increased RBC destruction, rather than exclusively rupturing of RBCs. There are two ways in which RBCs can be prematurely removed from the circulation or destroyed in vivo:
- Destruction of RBCs within blood vessels: Physical rupturing of the RBC membrane within vessels is called intravascular hemolysis. The hemoglobin is released into plasma (“free” hemoglobin), resulting in hemoglobinemia. Excess hemoglobin spills into the urine, resulting in hemoglobinuria.
- Phagocytosis of RBCs with destruction inside macrophages: This is called extravascular hemolysis, because it occurs outside vessels in the liver (Kupffer cells in the space of Disse, lining the sinusoids), splenic red pulp, and bone marrow stroma. This mode of RBC destruction does not involve direct rupture of RBC membranes within vessels, rather, the RBC is destroyed within the macrophage and the hemoglobin is metabolized within the macrophage and is not free in plasma (no hemoglobinemia or hemoglobinuria).
-
