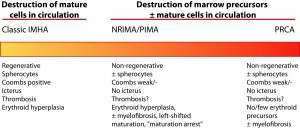
Immune-mediated anemia is a continuous spectrum of disease, ranging from the classical presentation of a regenerative hemolytic anemia with many spherocytes, positive Coombs test, hyperbilirubinemia (in some but not all animals) and erythroid hyperplasia in the bone marrow to the most severe clinical manifestation, a non-regenerative anemia due to the lack of RBC progenitors in the bone marrow or pure red cell aplasia (PRCA). Immune-mediated anemia can also present between these two extremes as either a weakly regenerative anemia or a non-regenerative anemia associated with bone marrow erythroid hyperplasia or hypoplasia. Erythroid hyperplasia is frequently characterized by left shifted erythroid maturation (more immature than mature erythroid progenitors in marrow), with fewer animals having erythroid maturation to a specific stage of erythropoiesis (“maturation arrest”). This is called ineffective erythropoiesis (a non-regenerative anemia in the face of erythroid hyperplasia indicates “ineffective” RBC production) and is presumed secondary to immune-mediated destruction of erythroid progenitors in the bone marrow or a precursor directed immune-mediated anemia (PIMA). Concurrent myelofibrosis is sometimes observed in the marrow as a consequence of the disease (not a cause of the syndrome). There is usually a lack of concurrent peripheral hemolysis (no spherocytes, negative Coombs test, no hyperbilirubinemia) in affected dogs, but some dogs can have both ineffective erythropoiesis and peripheral destruction. Dogs with classic IMHA (the regenerative variant) are frequently hypercoagulable (high fibrinogen, high D-dimer) and some are in concurrent disseminated intravascular coagulation. They are considered at risk of fibrosis. Hemostasis abnormalities and hyper coagulability do not appear to be as common in dogs with the non-regenerative forms of the anemia (PIMA or PRCA), however subsequent corticosteroid therapy can predispose all dogs to thrombosis. The pathological mechanisms underlying these different variations are unknown – it could be due to a combination of disease severity, different abnormalities in regulatory T cells, restricted expression of antigenic epitopes on specific RBC progenitors or other unknown factors.