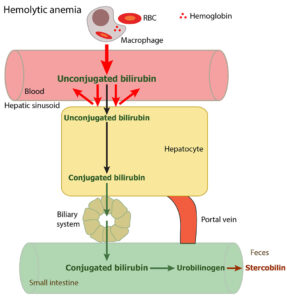
In a hemolytic anemia, increased amounts of unconjugated bilirubin are produced from excessive premature removal of RBCs, typically by extravascular hemolysis (intravascular hemolysis contributes a little to bilirubin production – the small proportion of free hemoglobin that is bound to haptoglobin is taken up by macrophages as the hemoglobin-haptoglobin complex, and the hemoglobin is degraded to unconjugated bilirubin; any unbound or free hemoglobin is excreted in the urine).
The unconjugated bilirubin binds to albumin and is taken up by hepatocytes. If (and only if) liver uptake cannot keep with production, unconjugated bilirubin concentrations will increase in blood (this depends on the rate and degree of hemolysis and underlying hepatic function, which can vary between animals). The unconjugated bilirubin that is taken up by the hepatocyte and conjugated is normally excreted into bile, although this can be in increased amounts, resulting in increased stercobilin and increased urobilinogen in urine (which is of no clinical consequence).
Bilirubinemia in animals with a hemolytic anemia is usually mostly due to unconjugated bilirubin (particularly if there are mild increases in total bilirubin) and there is no bilirubinuria – unconjugated bilirubin is water insoluble and cannot enter urine (plus the dipstick does not react with this form of bilirubin). This is also called prehepatic hyperbilirubinemia, indicating the bilirubin is coming from increased production by macrophages from removal of RBCs versus reflecting a hepatocellular or biliary issue. However, in some animals, the hemolytic anemia is complicated by cholestasis (for as yet unknown reasons) and then the picture and bilirubin split may change (see additional images).