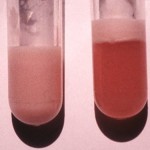
Lipid metabolism involves the interactions of lipoproteins, which enable the transport of lipids (triglycerides) in the circulation and uptake by tissues via specific receptors, and hormones that modify lipoproteins or control fat synthesis or breakdown. There are several different lipoproteins, with the main ones being chylomicrons (CM), very low density lipoproteins (VLDL), low density lipoproteins (LDL) and high density lipoproteins. These vary in their origin, triglyceride and cholesterol content, associated proteins (apolipoprotein) and role. All lipoproteins contain triglycerides and cholesterol in varying proportions. Visible or gross lipemia is usually caused by increases in the more triglyceride-rich lipoproteins (CM in particular but also VLDL). The most common cause of gross lipemia in dogs and cats (see image to the right) is not pathology but more of a collection-associated artifact or pre-analytical variable, which is collection of blood after eating – also called a post-prandial lipemia. Eating a diet with fat markedly increases CM and, thus, triglyceride concentrations (with minimal to no expected increase in cholesterol). Lipemia interferes with results of hematology and chemistry testing (see test basics, interferences, interference indexes) and should be avoided at all costs. Post-prandial lipemia can be minimized by collecting blood after a 12 hour fast in dogs and cats (see sample collection guidelines for hematology and chemistry), whereas blood sample collection in large animals does not require fasting or consideration of eating (this does depend on the analyte being measured or test that is being performed). Fasting lipemia in dog or a cat or visible lipemia in plasma or serum from large animals indicates an underlying lipid disorder (often called hyperlipemia or hyperlipidemia) and indicates an increase in CM or VLDL or a combination of both, with high triglyceride concentrations. A clue as to which lipoprotein class is increased can sometimes be obtained by looking at the supernatant plasma:
- Hypertriglyceridemia produces visible lipemia and indicates an increase in CM (usually) or VLDL. When hyperlipemia is from increased CM, e.g. postprandial hyperlipemia, CM will form a fat layer above a clear infranatant when serum or plasma samples are refrigerated. When hyperlipemia is due to increased VLDL, a fat layer does not form, but the sample may be cloudy, particularly if triglyceride concentrations are high (this is the main mechanism for visible lipemia in miniature horses and ponies with hyperlipidemia and camelids with negative energy balance). When there is a combination of both CM and VLDL, a fat layer will form above a cloudy infranatant. Note that very high concentrations of LDL may cause a slightly cloudy sample (no fat layer) due to increases in triglycerides (but cholesterol concentrations will be much higher)
- Hypercholesterolemia is generally caused by an increase in LDL and HDL (although high concentrations of VLDL and CM will also increase cholesterol, but not to the same extent as cholesterol – see classes below) and does not produce a visible hyperlipemia.
There can still be an increase in triglycerides (and of course cholesterol) in a given animal (small or large) without any visible lipemia.
Lipoprotein classes
- Chylomicrons (CM): These are the largest lipoproteins and contain about 90% triglyceride, 3% cholesterol and apolipoproteins B-48, C-II and E. They carry lipid from the gastrointestinal system to adipose tissue and skeletal muscle. Lipoprotein lipase, an enzyme located in the vascular endothelium, is activated by apolipoprotein C-II and hydrolyzes CM yielding fatty acids and glycerol and cholesterol-rich CM remnants. Fatty acids and glycerol are taken up by adipose tissue and skeletal muscle and re-converted into triglycerides for long-term fat storage. CM-remnants are taken up by the liver through remnant (apolipoprotein E) receptors where they are degraded into their lipid and protein components for other uses.
- Very low-density lipoproteins (VLDL): Very low-density lipoproteins contain about 62% triglycerides, 12% cholesterol, and apolipoprotein B-100, E and C-II. They are produced in the liver from free fatty acids. They are the main carrier of triglycerides in the fasting state, transporting triglycerides and cholesterol from the liver to peripheral tissues. This is accomplished by lipoprotein lipase on endothelial cells, which is activated by apolipoprotein C-II on VLDL and hydrolyzes VLDL liberating fatty acids, which are taken up by tissues. The removal of triglycerides forms a denser intermediate-density lipoprotein (IDL), which is then further hydrolysed to LDL. Some cholesterol-rich remnants of VLDL may be produced, which are taken up by remnant receptors in the liver .
- Low-density lipoproteins (LDL): Low-density lipoproteins contain approximately about 8% triglyceride, 42% cholesterol and apoliprotein B-100. LDL are responsible for delivering cholesterol to peripheral tissues, including the adrenal glands, ovary and testes, through LDL receptors. They are produced from VLDL by the action of lipoprotein lipase. LDL are removed from the circulation by the liver (with the help of hepatic lipase) and through LDL receptors on various tissues.
- High-density lipoproteins (HDL): High-density lipoproteins contain about 1-2% triglyceride, 30-36% cholesterol and apolipoprotein A, E and C. They are produced in the gastrointestinal system and the liver. They bind unesterified cholesterol released from tissues (with the help of the enzyme lecithin acylcholesterol transferase – LCAT). They are taken up by remnant receptors in the liver and are thus involved in reverse cholesterol transport (delivering cholesterol from peripheral tissues to the liver). Dogs differ from humans in that most of their cholesterol is carried as HDL versus LDL, and their LDLs have equal amounts of triglycerides and cholesterol. They also have different versions of HDL and their HDL are packaged differently (they have enzymes other than LCAT for modulating lipoproteins, since they do not seem to have much LCAT activity).
| Lipoprotein | Site of production | Content | Major apoprotein | Role | Effect (when increased)* |
| Chylomicron | Intestine | TG (90%) > chol (3%) | B-48 | Carry triglycerides (TG) from intestine (diet) to tissues. Major source of fat deposits. Acted on by endothelial lipoprotein lipase. Result in increased triglyceride concentrations. Think of them as the “exogenous” source of triglycerides. | Increased TG |
| VLDL | Liver | TG (62%) > chol (12%) | B-100 | Carry triglycerides from liver to tissues (supplying triglycerides to tissues for use for energy). VLDL are produced in the liver from non-esterified or free fatty acids liberated from fat stores after lipolysis is initiated by hormone-sensitive lipase. Acted on by endothelial lipoprotein lipase to generate IDL and LDL. Will increase triglyceride concentrations to a greater extent than cholesterol concentrations. Think of them as the “endogenous” source of triglycerides. | Increased TG and maybe cholesterol (TG > cholesterol) |
| LDL | Blood | Chol (42%) > TG (8%) | B-100 | Carry cholesterol (chol) to tissues for use by binding to LDL-receptors on cells. LDL are derived from VLDL after triglyceride is removed by endothelial lipoprotein lipase for tissue use. Removed from circulation in the liver by hepatic lipase and broken down to its constituent components. Increased LDL will increase cholesterol and possibly triglycerides (if LDL concentrations are high enough) but the increases in cholesterol will be greater than those of triglyceride. | Increased cholesterol and maybe triglycerides (cholesterol > TG) |
| HDL | Intestine, liver | Chol (∼30%) > TG (∼1%) (chol=TG in dog) |
A | Carry cholesterol to liver from tissues (“reverse” cholesterol”) transport. Increases in HDL will increase cholesterol concentrations. | Increased cholesterol |
| * The effect on triglyceride and cholesterol concentrations will depend on how much these lipoproteins are increased. Mild increases may not shift results outside of reference intervals. | |||||
The lipoprotein classes (VLDL, HDL, LDL) can be split into subfractions with polyacrylamide gel electrophoresis under non-denaturing conditions using a specific analyzer (Lipoprint, Quantimetrix) (Behling-Kelly et al 2022).
Hormones
The following hormones are involved in fat metabolism.
- Lipoprotein lipase (LPL): Lipoprotein lipase is found in vascular endothelium. It is activated by insulin, ACTH, TSH, glucagon and thyroid hormone. Its activity is enhanced by heparin. As discussed above, lipoprotein lipase hydrolyzes CM and VLDL to free (non-esterified) fatty acids and glycerol for tissue use. Cholesterol-rich remnants produced from both lipoproteins are removed by the liver. Lipoprotein lipase also converts VLDL to LDL (via IDL). Apolipoprotein C-II is essential for activation of LPL.
- Pancreatic lipase: Pancreatic lipase degrades dietary fat within the gastrointestinal lumen, allowing uptake and packaging into CM.
- Hepatic lipase: Hepatic lipase is an enzyme that hydrolyzes surface phospholipids on lipoproteins and is responsible for removing triglycerides from LDL (and helps the liver remove LDL from circulation).
- Hormone-sensitive triglyceride lipase: This enzyme is responsible for lipolysis (mobilization of triglycerides from adipose tissue to yield free or non-esterified fatty acids and glycerol). The enzyme is stimulated by catecholamines, glucagon, growth hormone, thyroxine, ACTH, corticosteroids and prostaglandins. It is inhibited by insulin (or the hormone is most active in the absence of insulin). Liberated non-esterified fatty acids are transported to the liver (free or albumin-bound), where they are taken up and used for energy (β-oxidation), re-combined with glycerol to form VLDL, or incorporated into ketones. Therefore, lipolysis will increase VLDL production (by providing the building blocks for production).
