Interpretation
Oxidant-induced hemolytic anemia
Explanation
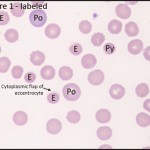
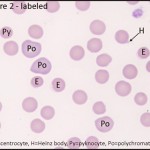
Based on the presence of polychromatophilic red cells (analogous to reticulocytes) on blood smear review, the anemia appears regenerative (confirmed by the high reticulocyte percentage and absolute reticulocyte count – see complete CBC results in Table 3 below). There are also moderate numbers of eccentrocytes with a few Heinz bodies and pyknocytes, which indicate a hemolytic anemia due to oxidant injury (see Table 2 below).
Discussion
Regenerative anemia can be caused by either blood loss or hemolysis. Therefore, patients with regenerative anemia should be assessed clinically for evidence of blood loss (e.g. trauma, dark stool, or severe ectoparasitism), and a blood smear should be assessed for evidence of the underlying cause of the regenerative anemia. With blood loss anemia, there may be no red cell morphologic changes on the blood smear other than polychromasia (except in cases of chronic blood loss leading to iron deficiency and red blood cell hypochromasia). However, with hemolytic anemias, there is often specific evidence of the underlying cause of the anemia that can be determined by evaluation of red blood cell morphology on the blood smear. Hemolytic anemias can be subdivided into five major categories: immune-mediated red blood cell destruction, oxidant injury, fragmentation injury, infectious diseases, and other miscellaneous causes (e.g. histiocytic disorders, inherited erythrocyte disorders, or severe hypophosphatemia). Examples of the common red blood cell abnormalities that can be used to diagnose each cause of hemolytic anemia are summarized in Table 2.
 |
 |
| Table 2: Red blood cell morphologic changes associated with various causes of hemolytic anemia | ||
| Red blood cell abnormalities most specific for the diagnosis | Less specific red blood cell abnormalities that may also be present | |
| Immune-mediated hemolytic anemia | Spherocytes, red blood cell agglutination | Polychromasia, nRBCs, siderocytes, target cells |
| Oxidant-induced hemolytic anemia | Eccentrocytes, Heinz bodies | Polychromasia, keratocytes, pyknocytes |
| Fragmentation anemia | Schistocytes, acanthocytes, keratocytes | +/- polychromasia (often less regenerative than other causes of hemolytic anemia); some schistocytes may resemble spherocytes |
| Infectious hemolytic anemia | +/- Erythroparasites (Mycoplasma, Babesia, Anaplasma, etc.) | No abnormalities are seen in some cases, especially if anemia is caused by viruses (e.g. Equine infectious anemia) or bacteria (e.g. Leptospirosis) |
| Other (miscellaneous) | Variable | Variable |
Eccentrocytes can look similar to spherocytes in that they are often smaller and darker than normal red blood cells. The distinguishing feature of eccentrocytes is the clear cytoplasmic flap on one side of the cell that represents oxidant-induced fusion of the cell membrane. In some cases, this flap is not visible because it is either tucked under the cell or has been removed by the spleen (the resultant red blood cell is termed a pyknocyte). The presence of frequent eccentrocytes and a few Heinz bodies in this dog (see labeled images below) indicates that his anemia is caused or complicated by oxidant-injury. Eccentrocytes and/or Heinz bodies have been described to occur in a numbers of conditions in dogs, including ingestion of certain foods, drugs, or chemicals, such as: onions, garlic, acetaminophen, benzocaine, propofol, zinc, naphthalene (in moth balls), vitamin K antagonist rodenticides, and others.1-3 Additionally, eccentrocytosis has also been reported in dogs with T cell lymphoma, diabetes mellitus, and in dogs given whole blood transfusions.1
| Table 3: Complete CBC results | |||
| Test | Results | Units | Ref interval |
| Hct | 27 L | % | 41 – 60 |
| Hgb | 8.6 L | g/dL | 14.1 – 20.2 |
| RBC | 3.5 L | mill/μL | 5.7 – 8.6 |
| MCV | 77 H | fl | 66 – 76 |
| MCH | 25 | pg | 22 -26 |
| MCHC | 32L | g/dL | 33 – 36 |
| RDW | 15.4 H | % | 10.6 – 14.4 |
| Retic % | 5.4 H | % | 0.2 – 1.5 |
| Retic Abs | 189.8 H | thous/μL | 11.1-94.7 |
| nRBCs | 10 | /100 WBC | 0 – 1 |
| WBC | 8.7 | thous/μL | 5.7 – 14.2 |
| Seg | 6.5 | thous/μL | 2.7 – 9.4 |
| Band | 0.1 | thous/μL | 0 -0.1 |
| Lymph | 1.5 | thous/μL | 0.9 – 4.7 |
| Mono | 0.4 | thous/μL | 0.1 – 1.3 |
| Eos | 0.1 | thous/μL | 0.1 – 1.3 |
| Baso | 0.0 | thous/μL | 0 – 0.1 |
| Plat | 278 | thous/μL | 186 – 545 |
| MPV | 18.3 H | fl | 8.4 – 14.1 |
| TP-ref | 7.5 | g/dL | 5.9 – 7.8 |
| RBC exam: Mild anisocytosis, moderate eccentrocytes, few Heinz bodies, mild polychromasia | |||
| Parasites: None seen | |||
| WBC exam: No significant abnormalities | |||
| Plasma appearance: Normal | |||
Follow up
In this case, the cause for the oxidant injury was not specifically identified. To rule out other causes contributing to the regenerative anemia, additional testing was performed including a Coomb’s test (negative), fecal parasite exam (negative), a coagulation profile (within normal limits), and blood lead and zinc levels (low).
No specific treatments were administered. The dog’s pack cell volume was re-checked on a weekly basis, and had increased to 39% after one week, and to 49% after two weeks. The resolution of the anemia without specific treatment supports that the oxidant-induced hemolytic anemia in this dog was caused by a single exposure to an exogenous oxidant, perhaps in the garage. Depending on the severity of the clinical signs and the underlying cause of the oxidant injury, more specific treatment may be needed in some cases (e.g. antioxidants, N-acetylcysteine, transfusions, etc.).
References
- Caldin M, Carli E, Furlanello T, et al. A retrospective study of 60 cases of eccentrocytosis in the dog. Vet Clin Pathol. 2005;34:224-231.
- Houston DM, Myers SL. A review of Heinz-body anemia in the dog induced by toxins. Vet Hum Toxicol. 1993;35:158-161.
- Desnoyers M, Hebert P. Heinz body anemia in a dog following possible naphthalene ingestion. Vet Clin Pathol. 1995;24:124-125.
