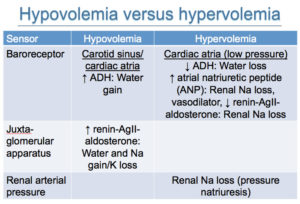
Baroreceptors in the carotid sinus (high pressure) and left atria (low pressure) respond to decreases in effective circulating volume (hypovolemia) by stimulating ADH release, which causes water without sodium retention in the kidneys. Catecholamine release is also stimulated and causes sodium and water absorption in the proximal tubules of the kidney and vasoconstriction as well as stimulation of renin release. Decreased arterial pressure in the afferent arteriole of the glomerulus stimulates the renin-angiotensin-aldosterone system, which causes sodium and water absorption in the distal nephron (aldosterone) and proximal tubules (angiotensin) and thirst (water intake without sodium, in response to angiotensin).
Conversely in states of hypervolemia, low pressure receptors in the cardiac atria inhibit ADH, leading to water loss, increase atrial natriuretic peptide, which may function primarily through causing vasodilation but also stimulates sodium loss in the kidneys as well as inhibition of the renin-angiotensin-aldosterone system, leading to renal and water loss. In the kidneys, there is a pressure-induced natriuresis, which may be the main mechanism resulting in sodium and water loss and correction of hypervolemia.