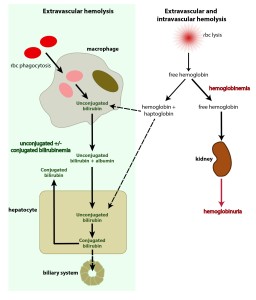
This schematic depicts the sources of bilirubin and what may occur in hemolytic anemia. The main source of bilirubin (depicted by thick arrows and green shaded rectangle) is removal of RBCs (e.g. with antibody or complement attached to them, such as in an immune-mediated anemia) by macrophages in the spleen and other organs. The phagocytized RBCs are broken down and the heme group in hemoglobin converted to unconjugated bilirubin. This is then exported from the macrophage, binds to albumin and is taken up by hepatocytes. Once in the hepatocyte, the bilirubin is conjugated and excreted into bile. When more unconjugated bilirubin is produced by the macrophages than the liver can handle, unconjugated bilirubin builds up in blood, leading to high total bilirubin values. This is the common scenario in large animals with hemolytic anemia and in many dogs and cats, particularly when the bilirubin concentration is low. However, in some dogs and foals with neonatal isoerythrolysis, they develop a defect in bilirubin excretion into bile (shown by the dashed arrow) and conjugated bilirubin that builds up (remember more is being produced as it is building up) gets “regurgitated” back into blood, leading to high conjugated bilirubin, which may exceed unconjugated bilirubin in amount. When there is an intravascular component to the hemolysis (e.g. membrane attack complex of complement assembles on RBCs, rupturing their membranes, or a parasite such as Babesia exits the cell, rupturing as it goes), the hemoglobin is liberated into the circulation, resulting in hemoglobinemia. Some of this free hemoglobin binds to proteins called haptoglobulin (shown) and hemopexin and the hemoglobin complexed to these proteins is taken up by macrophages and hepatocytes, who have receptors for the binding proteins (e.g. CD163 for haptoglobin). Both the macrophage and hepatocyte can then convert the hemoglobin to unconjugated bilirubin, but since most of the free hemoglobin is actually filtered through the kidneys and “lost” in the urine (hemoglobinuria), this contributes only a small amount to the total bilirubin (unconjugated or conjugated) that is being formed, with the vast majority coming from the extravascular hemolysis, which is concurrently occurring. Thus, an intravascular component to a hemolytic anemia can be recognized by hemoglobinemia and hemoglobinuria which will be absent if the anemia is only due to extravascular hemolysis. Note, that for simplification, we have not shown the conjugated bilirubin being excreted in the urine in the above schematic. When conjugated bilirubin increases in blood, it is rapidly spilled into urine (as it is water soluble), so a bilirubinuria precedes an increase in total bilirubin when conjugated bilirubin is increased (and bilirubinuria indicates cholestasis in all species, other than dogs, in which small amounts of bilirubin can be present in the urine of healthy dogs, particularly males, without cholestasis).