WBC count
The white cell count (WBC) is the total number of leukocytes in a volume of blood, expressed as thousands/µL. As with the RBC, the WBC can be done by manual methods or by automated cell counters. The WBC by any method is a count of nuclei or total nucleated cell count. If nucleated red blood cells (nRBC) are circulating in blood, they will be included in the nucleated cell count whether the count is done by manual methods or by automated analyzers. In such cases, the WBC represents the leukocyte count only after it has been corrected for the nucleated red cells (nRBCs). The number of nRBCs per 100 leukocytes is recorded during the differential leukocyte count. Then a correction is made as follows:
Corrected WBC = nucleated cell count x [100 ÷ (nRBC + 100)]
In reports from the Clinical Pathology Laboratory of Cornell University (excluding automated hematology tests), the WBC value is usually a leukocyte count on our routine mammalian hemograms, since we correct for the presence of nRBCs if > 5 nRBCs are counted in a 100 cell differential leukocyte count.
Method of measurement
Any of these methods of white blood cell determination counts nuclei not actually WBC. Thus, we often refer to the count as nucleated cell count, which in most cases of mammalian blood (which contains low numbers of nucleated RBC), is synonymous with the white blood cell count. Since exotic animals (reptiles, birds, fish) have nucleated everything (RBC, WBC, platelets), we have to use a different technique to count their WBC.
- Manual hemocytometer counts: The manual procedure, using a diluting chamber and a hemocytometer, is no longer used except for white cell counts in body fluids with extremely few cells (< 1,000 cells/µL), e.g. cerebrospinal fluid. It involves diluting blood in a diluent that lyses the red cells to remove them from view. A hemocytometer is charged with the diluted blood and nuclei are counted in the appropriate areas of the grid using a light microscope. The manual WBC is a reasonable test to do in-office since it is not terribly time- and labor-intensive and gives acceptably accurate results.

- Impedance counters: Laboratories use either impedance-based electronic cell counters to generate WBC counts in body fluids and non-EDTA samples. In our laboratory, the Coulter Z2 (a bench-top impedance counter) is our back-up analyzer. We use this cell counter when our regular hematology analyzer is out of commission or a sample other than EDTA-anticoagulated blood is submitted for cell counts. This is the standard instrument used for cell counts (total nucleated and red blood cell count) in body fluids, other than blood, e.g. joint fluids, peritoneal fluids, because these fluids cannot be analyzed through the automated hematology analyzer.
- Flow cytometry counters: We use the hematology analyzer, the ADVIA 2120, to obtain WBC counts. This analyzer counts WBC in two ways, both of which use laser light: the peroxidase method and the basophil method.

-
- Peroxidase method: White blood cells are stained with peroxidase and the cells are counted based on size and staining characteristics. The analyzer also provides an automated differential cell count by separating the cells into clusters, using the peroxidase channel. The peroxidase method will give falsely high counts in samples with numerous platelet clumps. This type of artifact is also prominent with impedance-based counters, resulting in erroneously high WBC counts in certain species, especially cats (whose platelets are prone to clumping).
- Basophil method: The basophil method involves stripping the cells of cytoplasm and counting nuclei. In this cytogram, the cells are displayed as a worm, with the mononuclear cells (lymphocytes and monocytes) in the head and the granulocytes (neutrophils) in the body of the worm. This is a far more accurate method for counting white cells and is the default method on the ADVIA.
-
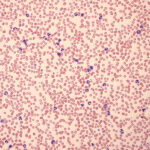
Increased leukocyte count Smear estimate: The least accurate, by far, of all the methods for counting leukocytes, nevertheless this may be the only method available if a sample has clotted but a blood smear made before clotting is available. Estimates vary depending on source and are dependent on the smear being well made and from an appropriate volume of blood (making too thin a smear will result in an underestimate). The leukocytes also need to be well-spread and not concentrated at the feathered edge. This guideline can be used for estimation with the above caveats:
- Average of 1 leukocyte/50x oil immersion field using a 10x eyepiece = 2 – 2.5 thousand leukocytes/µL. This works well for avian blood.
- Average of 1 leukocyte/40x high dry field using a 10x eyepiece = 2.5-3.1 thou/µL.
- Average around 10 fields
- Examine the smear first on low magnification (1ox objective) to find the monolayer and evaluate even leukocyte distribution and number of cells at the feathered edge and in the thicker parts of the smear.
Test interpretation
- Artifact: A falsely increased WBC count in the basophil channel (the default method on the ADVIA) can be seen in rare cases of cats with Heinz bodies (>50% RBCs) (Dondi et al 2019). Falsely decreased WBC counts can be seen with any analyzer as a storage artifact (as cells swell and lyse) or with fragile lymphocytes, which occurs in rare cases of chronic lymphocytic leukemia.
- Increased WBC count (leukocytosis)
This in itself is not meaningful, because interpretation depends on what type of leukocyte is increased. A leukocytosis due to a neutrophilia has a far different meaning than a leukocytosis due to a small lymphocytosis. The former could be due to inflammation, corticosteroids or epinephrine while the latter could be due to antigenic stimulation, lymphoma or a chronic lymphocytic leukemia. For more information, see related links below on individual leukocyte changes and leukogram patterns (under leukogram changes). - Decreased WBC counts (leukopenia)
As indicated above, a WBC should never be interpreted alone, but should be interpreted with respect to the changes in the individual leukocytes that comprise the WBC count. For instance, a mild leukopenia due to a lymphopenia may signify a stress leukogram, whereas a mild leukopenia that is due to neutropenia with a degenerative left shift (more bands than segmented neutrophils) indicates severe inflammation. Toxic change usually is seen in neutrophils (and band forms) in the latter situation and indicates accelerated or premature release (neutrophil immaturity) in response to the inflammation. A special situation is when the WBC count is decreased due to a neutropenia and there is a concurrent non-regenerative anemia and thrombocytopenia. This is called pancytopenia and is caused by specific mechanisms, such as bone marrow aplasia, hematopoietic neoplasia (leukemia), and drug toxicities.
Differential WBC count
This is usually done manually by counting 100 leukocytes in the monolayer of the smear, which provides relative proportions (percentages) of WBC normally found in blood. During a differential count, leukocytes are separated into general categories, including neutrophils (mature segmented cells), bands (all stages of immature neutrophils, indicating the presence of a left shift), lymphocytes (any size, including reactive cells), monocytes, eosinophils and basophils. At Cornell University, we also include a category of “Other WBC” which includes hematopoietic cells that are not normally seen in blood, e.g. mast cells, blasts associated with a leukemia. The percentage of each cell type is then converted to an absolute count (thousands/uL) by multiplying the percentage by the total WBC count (after accounting for nucleated red blood cells as indicated above). Some laser-based hematology analyzers can also give an automated differential leukocyte count (see above), which is accurate for neutrophils, lymphocytes and eosinophils (in some species), but less so for other leukocytes.
Test interpretation
A differential count should never be interpreted in percentages but should always be interpreted with respect to the total WBC count. For instance, 30% eosinophils in an animal with a low normal WBC may not be an increase in absolute eosinophil count (i.e. an eosinophilia) but would certainly be called an eosinophilia if the WBC count was 20,000/uL (equating to 6,000/μL eosinophils). See individual WBC for more information on changes in each leukocyte.
