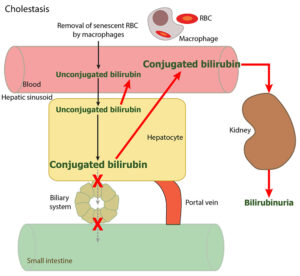
Cholestasis indicates decreased or ceased bile (and conjugated bilirubin) flow. This can occur due to structural compression of biliary canaliculi or defective bile/bilirubin transporter function (e.g. secondary to inflammatory cytokines) (upper red X) or a structural blockage to bile flow at the level of the bile duct, gall bladder or intestine (where the bile duct enters the intestine). A ruptured gall bladder also results in cholestasis (note any form of structural cholestasis also results in downregulation of the transporters that move bile/bilirubin from the hepatocyte to the biliary canaliculi).
Lack of excretion of conjugated bilirubin into the intestine results in pale-colored feces (reduced or no production of stercobilin). The conjugated bilirubin that is no longer being excreted into the intestine is refluxed back into blood (via reversal of transporters) and freely filtered by the glomerulus into the urine, because it is water soluble and overcomes renal resorptive capacity quickly (low renal threshold). Cholestasis can be recognized by a bilirubinuria that is excessive for a urine specific gravity (USG) in a dog or a bilirubinuria in any USG in other species.
Conjugated or direct bilirubin concentrations will increase in blood with cholestasis, but bilirubinuria will precede a direct bilirubinemia in early developing cholestasis. Unconjugated bilirubin also increases in blood in cholestatic conditions due to reversal of transporters that normally take it up and secondary liver injury from accumulated bile salts, which emulsify membranes. However, direct bilirubin concentrations usually exceeds indirect (unconjugated) bilirubin concentrations in blood in animals with cholestasis.
Note that unconjugated bilirubin production is normal in cholestasis because there is no hemolytic anemia present and only normal senescent RBCs are being removed and contributing to unconjugated bilirubin production, as they would normally.