Interpretation
Marked neutrophilic/histiocytic (pyogranulomatous) inflammation with intralesional yeast consistent with Blastomyces dermatitidis
Explanation
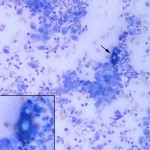
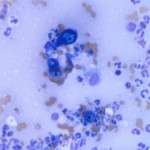
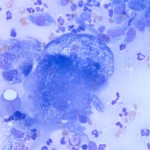
The cytology smears are highly cellular consisting of many mixed inflammatory cells and low numbers of large broad-based budding yeast. The yeast are approximately 15-20 um in diameter, deep green-blue to royal blue with a thick refractile double-contoured cell wall and slightly granular internal complexity (Figures 2 and 3). The mixed inflammatory cells are predominantly non-degenerate to mildly degenerate neutrophils with fewer macrophages. Numerous fibroblasts (spindle-shaped cells) are also present. Low numbers of multinucleated giant cells with up to 20 evenly-sized nuclei (“foreign body-type cells”) are also noted (Figure 4). Whenever this pattern of inflammatory cells is observed, an exogenous or endogenous foreign body reaction or infectious agent (e.g. fungi, protozoa) are considered as the main differential diagnoses for inciting cause.
Discussion
Blastomycosis is caused by a dimorphic fungus with an environmental saprophytic mycelial form (Ajellomyces dermatitidis) that reproduces sexually producing infective spores that transform into asexually reproducing yeast (Blastomyces dermatitidis) at body temperature1. The reservoir for Blastomyces is thought to be the soil and the organism requires a sandy, acidic soil and proximity to water for growth. Indeed, involvement in dirt-moving activities and proximity to water are risk factors for blastomycosis. A study in Louisiana dogs found that dogs with blastomycosis were 10 times more likely to live within 400 m of water than control dogs2. Geographically, Blastomyces is distributed throughout the Mississippi, Missouri, and Ohio River valleys, the Mid-Atlantic States, and the Canadian provinces of Quebec, Manitoba, and Ontario. Several cases have also been identified originating from a region of the Adirondack Mountains in upstate New York3. Dogs and people are most commonly affected, although infections in various domesticated and wild species have been reported, and dogs appear to be more susceptible to infection than people. Most cases of blastomycosis are systemic with the route of entry via inhalation. From the lungs, the yeast disseminate throughout the body with preferred sites including the skin, eyes, bones, lymph nodes, and subcutaneous tissues. Intestinal lesions are uncommon in dogs with systemic disease. Solitary lesions occasionally develop via puncture wounds, but localized lesions should be considered part of a systemic process until proven otherwise. Clinical signs of blastomycosis in dogs include anorexia, weight loss, cough, dyspnea, ocular disease, lameness, and skin lesions. The majority (approximately 85%) of dogs with blastomycosis will have lung changes (nodular or interstitial pattern) on thoracic radiographs, and up to 40% will have ocular lesions (most commonly uveitis)1. Common laboratory abnormalities include a mild non-regenerative anemia (anemia of inflammatory disease), mild hypoalbuminemia (negative acute phase response), and hyperglobulinemia due to a polyclonal gammopathy (chronic antigenic stimulation) and/or an increase in the α2-globulins (positive acute phase response). A definitive diagnosis is made cytologically or histologically based on the characteristic “big blue broad-based budding” morphology of the yeast form. Serologic testing is available, but has mediocre sensitivity and false negative results are common1. Recently, an enzyme immunoassay (EIA) for the detection of Blastomyces antigen in urine and serum has been evaluated and has good sensitivity in urine, but the specificity of this assay for the detection of Blastomyces antigen from other mycoses was not sufficiently evaluated in this study4. Cross-reaction of this assay with other mycoses, such as Histoplasma capsulatum, occurs in human medicine5 and similar cross-reactivity is likely in dogs.
Further information and follow-up
The patient had no relevant abnormalities on a complete blood count, biochemical panel, or urinalysis. Thoracic radiographs were unremarkable. Mild anterior uveitis was noted on ophthalmologic examination. Fungal serology was negative. A diagnosis of localized blastomycosis, likely via a puncture wound to the paw, was made based on lack of evidence of systemic disease. The patient was prescribed systemic antifungal medication as well as ophthalmic non-steroidal anti-inflammatory drops for the uveitis. At recheck examination one month post-diagnosis, the owners reported marked improvement in the patient’s weight-bearing on the affected paw. On physical examination, there was mild thickening of the skin between the pads of digits III and IV on the left rear paw, but no swelling, pain, or redness was noted. On ophthalmologic examination, the anterior uveitis was controlled. Bloodwork was unremarkable. The patient was discharged with a plan to continue all medications until the next recheck examination.
References
- Legendre AM. Blastomycosis In: Greene CE, ed. Infectious Diseases of the Dog and Cat. St. Louis, Mo; Saunders Elsevier, 2006;569-576.
- Arceneaux KA, Taboada J, Hosgood G. Blastomycosis in dogs: 115 cases (1980-1995). J Am Vet Med Assoc 1998;213:658-663.
- Cote E, Barr SC, Allen C, et al. Blastomycosis in six dogs in New York State. J Am Vet Med Assoc 1997;210:502-504.
- Spector D, Legendre AM, Wheat J, et al. Antigen and antibody testing for the diagnosis of blastomycosis in dogs. J Vet Intern Med 2008;22:839-843.
- Durkin M, Witt J, LeMonte A, et al. Antigen assay with the potential to aid in diagnosis of blastomycosis. J Clin Microbiol 2004;42:4873-4875.